About tubular cells
For the routine examination, the different renal tubular epithelial cells are regrouped under the term: renal cells. This term implies several types of cells. As it has been mentioned, it is impossible to know with confidence the origin of a tubular cell without using a sophisticated method, like staining specific markers with conjugated monoclonal antibodies.
Schumann has described some particular tubular cells based on usual microscopic characteristics. The cells described are: the convoluted proximal tubular cells (convulted RTC2), the collecting duct renal tubular cells (collecting duct RTC), the necrotic renal tubular cells (necrotic RTC) and finally the epithelial fragments.
In a wet preparation, the distinction between some tubular cells and the leukocytes is not always obvious. To be able to evaluate the number of tubular cells in a specimen with a marked leukocyturia, the naphtyl AS-D chloroacetate esterase is used.
Proximal renal tubular cells
 This cell is described by Schumann
as a large size cell (20 to 60 m) with an abundant granular
cytoplasm, and a blunted cell membrane. The nucleus is round and
eccentric. In a wet preparation and under bright field
microscopy, this cell can easily be confused with a small
granular cast. The proximal tubular cells are known to have an
elaborate brush border. This fragile structure is constructed
from folds of the cellular membrane. In a toxic or ischemic
state, the brush border is eliminated and is found in the urine
in the form of granules. These granules can be free, but can also
be embedded in a cast matrix (granular casts).
This cell is described by Schumann
as a large size cell (20 to 60 m) with an abundant granular
cytoplasm, and a blunted cell membrane. The nucleus is round and
eccentric. In a wet preparation and under bright field
microscopy, this cell can easily be confused with a small
granular cast. The proximal tubular cells are known to have an
elaborate brush border. This fragile structure is constructed
from folds of the cellular membrane. In a toxic or ischemic
state, the brush border is eliminated and is found in the urine
in the form of granules. These granules can be free, but can also
be embedded in a cast matrix (granular casts).
The exfoliated proximal tubular cell undergoes many changes, due to the travel in the osmotic changing environment, from the proximal tubule to the bladder . It is unlikely to find these cells intact.
Collecting duct renal tubular cells
 The collecting duct renal tubular
cells are originally of a cubic shape; but once exfoliated, these
adopt a rounded shape. These cells are slightly larger than
leukocytes (10-14 mm) with a lightly
granular cytoplasm. The nucleus is round and well defined (due to
the thick nuclear membrane) and usually centric. The cytoplasm
shows a perinuclear halo, when stained or under phase contrast.
The collecting duct renal tubular
cells are originally of a cubic shape; but once exfoliated, these
adopt a rounded shape. These cells are slightly larger than
leukocytes (10-14 mm) with a lightly
granular cytoplasm. The nucleus is round and well defined (due to
the thick nuclear membrane) and usually centric. The cytoplasm
shows a perinuclear halo, when stained or under phase contrast.
The RTC casts are frequent with high exfoliation specimens. This fact can be of help for identification, since the similarities between the free cells and the cast cells should be evident.
These cells are the most frequently observed renal tubular cells. With the cytodiagnostic method, Schumann has reported a normal value of less than 20 cells per 10 fields at hpf. Values of over a 100 cells/10 x hpf is indicative of a renal parenchym disease. For the routine analysis, a value of less than 1 cell/hpf (a few cells) is a normal expected value.
Necrotic renal tubular cells
The necrotic renal tubular cell is an important element of Schumann cytodiagnostic method. This cell is described, with the PAP stain, as ghost cells, with the form and size of normal cells, and with poorly stained nuclei. The cytoplasm of these cells is highly granular.
 Due to
special conditions, the collecting duct renal tubular cells are
unable to resist to the low osmolality of the urine. As water and
salts get in the cells, the cytoplasm starts to disorganize. The
cell swells, the cytoplasm takes a granular aspect and the
nucleus shrinks and becomes pycnotic. At the end of the process,
the cells are completely granular. The granules are quite similar
to those found in granular casts (it is frequent to observe
identical granules in cells and in casts).
Due to
special conditions, the collecting duct renal tubular cells are
unable to resist to the low osmolality of the urine. As water and
salts get in the cells, the cytoplasm starts to disorganize. The
cell swells, the cytoplasm takes a granular aspect and the
nucleus shrinks and becomes pycnotic. At the end of the process,
the cells are completely granular. The granules are quite similar
to those found in granular casts (it is frequent to observe
identical granules in cells and in casts).
In an acute tubular necrosis of ischemic origin, granules in renal tubular cells and in granular casts (dirty brown cast) bare the same dark red-brown pigmentation. The pigments are related to hemoglobin and methemoglobin.
Renal epithelial fragments
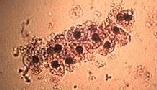 For Schumann,
renal epithelial fragments have a high clinical value. The renal
epithelial fragments are quite different from cell clusters. The
epithelial fragment is a piece of tissue. It is not normal to
have tissue fragments in urine.
For Schumann,
renal epithelial fragments have a high clinical value. The renal
epithelial fragments are quite different from cell clusters. The
epithelial fragment is a piece of tissue. It is not normal to
have tissue fragments in urine.
The fragments are described as a structure of at least three tubular cells with an intercellular cohesion. The distinction between fragments and renal tubular cell casts is not always easy. This identification can be made on the basis of the presence, or not of a matrix. The renal epithelial fragments also have to be distinguished from the urothelial fragments. The identification is made upon cellular criteria.
Schumann has proposed criteria, characteristics to renal epithelial fragments.
| Characteristics of Renal Epithelial Fragments Found in Urine Sediment |
|---|
| Configuration characteristics
of a renal epithelium
Encasement of casts Cylindrical (sleeve-like) arrangement Sheets with "honeycomb"arrangement Spindle or elongated cells |
| Additional characteristics of a renal epithelium
Encasement of crystals Intracytoplasmic lipid Intracytoplasmic cast material |
In histological cut sections, fragments are associated to ruptures of the basement membrane at the collecting duct level. The presence of epithelial fragments must always be considered as abnormal. Schumann has reported characteristic epithelial fragments in: acute tubular necrosis (5 cases), renal allograft reject (20 cases), papillary necrosis (2 cases) and renal infarction (12 cases). (original in Acta cytol 25:147-152, 1981)
Renal cells and fragments from the terminal section.
 In some cases, one can find, in a specimen, isolated
cells fragments that originate from the terminal part of the
large tubes (tubes of Bellini). These large tubes are lined with
a cylindrical epithelia, and form the urinary canal of the
papilla. Considering the proximity of the region, and due to the
fact that at this level the urine is no longer modified, isolated
cells and fragments can have a well preserved morphology. These
cells have an average size of (20 - 30 mm)
and are round or clearly cylindrical; the nuclei are eccentric in
the cylindrical cells. The presence of some rare cells of this
type can be considered as a normal renewal.
In some cases, one can find, in a specimen, isolated
cells fragments that originate from the terminal part of the
large tubes (tubes of Bellini). These large tubes are lined with
a cylindrical epithelia, and form the urinary canal of the
papilla. Considering the proximity of the region, and due to the
fact that at this level the urine is no longer modified, isolated
cells and fragments can have a well preserved morphology. These
cells have an average size of (20 - 30 mm)
and are round or clearly cylindrical; the nuclei are eccentric in
the cylindrical cells. The presence of some rare cells of this
type can be considered as a normal renewal.
These cells can represent an identification difficulty.
While being renal cells, in the routine microscopy, these are reported as an urothelial cells. These cells are often found in various urological problems like in obstruction, urolithiasis and others. In the presence of similar cells or fragments, without cast, this type of urothelial cells should be considered.